
Sally Morrow
Senior Moving and Handling Adviser at Manchester Foundation Trust with 23 years experience within the NHS as a Physiotherapist

Senior Moving and Handling Adviser at Manchester Foundation Trust with 23 years experience within the NHS as a Physiotherapist
Lateral transfers, the task of moving a supine patient horizontally between two adjacent surfaces, is a frequent activity in healthcare and is reported to be the most common cause of back and shoulder injuries in nursing staff due to the considerable physical demands involved.
Friction-reducing devices (FRDs) were developed with the aim of easing the physical burden on handlers when repositioning patients in bed and have been shown to be beneficial in reducing the risk of injury. Studies have acknowledged that the firmness of a surface upon which a patient is lying, appears to be an important factor in determining the forces required to perform a lateral transfer with a FRD and the purpose of this study was to explore that idea.
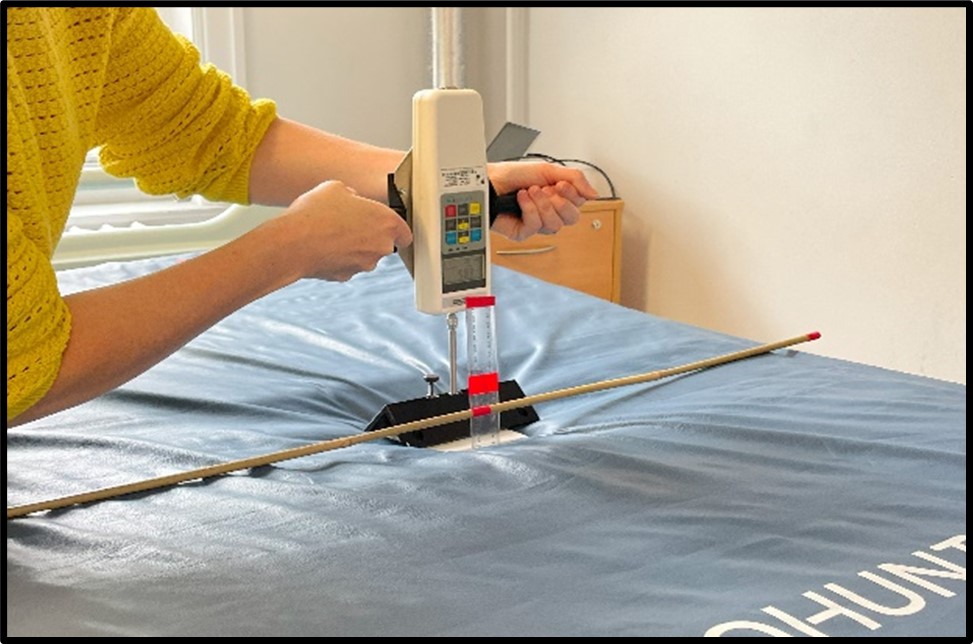
Split into two stages, this study adopted a repeated measures design to establish the co-efficient of friction between 5 clinical surfaces and 5 popular FRDs. The firmness of the surfaces were measured using a modified Indentation Load Deflection test and the peak hand forces required to move a subject across those surfaces on each FRD were recorded
Experienced patient handlers (n=16) then performed a series of lateral transfers using 3 FRDs across 5 surfaces, recording peak hand forces and self reported Rates of Perceived Force (RPF) to determine the physical demands experienced.
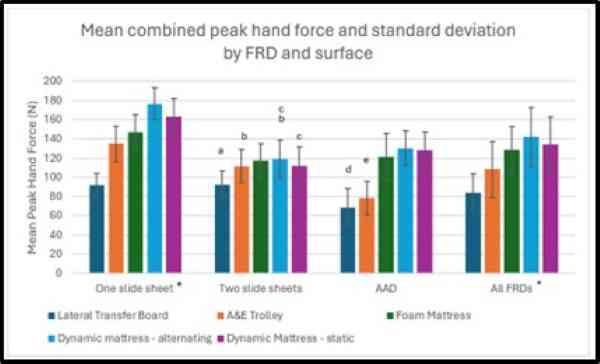
This study found there is an inversely proportional relationship between surface deflection and co-efficient of friction, with a strong negative correlation but this effect is minimised by use of slide sheets. There was a significant difference in peak hand force across each surface when FRDs are considered as a whole, but when grouped by FRD, any significant difference in hand forces were dependent on the combination of FRD and surface deployed. Differences in peak hand force were not mirrored by self-reported perceptions of force due to methodological challenges.
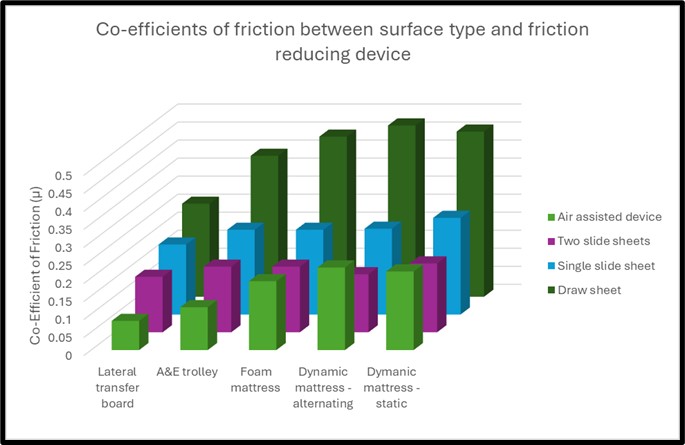
There is clear evidence that the surface upon which a patient is lying has a significant effect on the physical demands placed on handlers performing lateral transfers. The firmer the surface, the easier it is to move a patient across it using a FRD.
The literature supports the use of air-assisted devices for lateral transfers but this study suggest this is only true on firmer surfaces and that two slide sheets are more effective at reducing physical demand as they appear to negate the effect of friction across a wide range of surfaces.

Findings from this study suggest that air-assisted devices are recommended for use on firm surfaces such as theatre tables and A&E trolleys, but on softer surfaces like foam and air mattresses, two slide sheets are more effective in reducing the physical demands placed on handlers. This makes slide sheets a very appealing solution for use in any clinical setting where patients are nursed in hospital beds, with great benefits in terms of safety, standardisation, training and cost reduction.
The findings of this study also provides some rationale for common clinical practises such as using slide sheets as a pair rather than singularly, avoiding the use of draw sheets and placing alternating dynamic mattresses on static before commencing any patient repositioning on the bed.
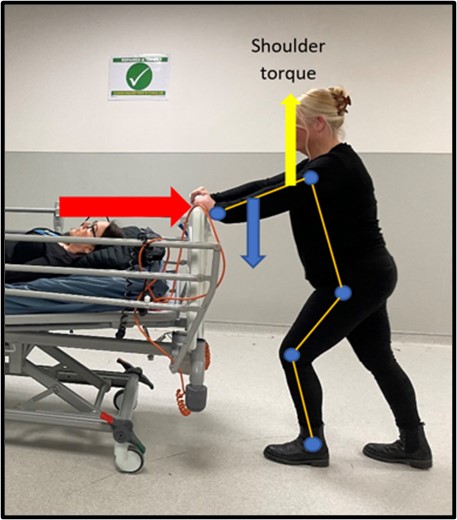
Physical Ergonomics: Postural analysis using Ovako Working Posture Analysing System (OWAS) and Rapid Entire Body Assessment (REBA), along with physiological and biomechanical analysis were undertaken for an ergonomic analysis of bed pushing. Anthropometrics analysed the suitability of the equipment for the operator and consideration was given to the problems this poses for hospital porters. The evaluation established bed pushing as a high risk activity for porters and appropriate risk-reduction measures were suggested.

Patient Handling: The ergonomics of lifting the fallen patient were studied by analysing two methods of flat lifting within a hospital setting. Task analysis mapped the system of work for falls retrieval at the participating Trust and identified lifting as a high risk activity. An ergonomic evaluation of a manual flat-lift using a scoop stretcher was then compared to an air assisted flat-lifting device via postural analysis using REBA, biomechanical and physiological analysis and recommendations for safe systems of work were made. This ergonomic evaluation has provided evidence for the implementation of air assisted flat-lifting devices in the participating Trust.

Patient Safety: A systems analysis was undertaken to analyse a hoist maintenance system within an acute hospital. Systems Engineering Initiative for Patient Safety (SEIPS 2.0) was used to provide an overview of the work system whilst swim lane analysis and Systems Theoretical Accident Model and Processes (STAMP) models mapped the process and control structures in place. Failure Modes and Effects analysis (FMEA) identified inherent risks within the system. Risk mitigation and resilience control measures were recommended for implementation, prioritised by the NIOSH Hierarchy of Control.